For the umpteenth time in recent memory, the gates of the Lagos University Teaching Hospital (LUTH) swung shut again to the thousands of patients who rely on the nation’s tertiary centers. The announcement by the Joint Health Sector Unions (JOHESU) and the Assembly of Healthcare Professional Associations of an indefinite nationwide strike was not just a headline; it was a life-threatening reality.
The industrial action, triggered by the federal government’s delay in implementing the revised Consolidated Health Salary Structure (CONHESS), has once again disrupted medical services nationwide, underscoring a systemic vulnerability: Nigeria’s health economy is currently hostage to centralisation.
Nigeria’s medical sector has experienced frequent industrial actions over the past decade, primarily driven by disputes over the Consolidated Medical Salary Structure (CONMESS) for doctors and the Consolidated Health Salary Structure (CONHESS) for other health workers, unpaid arrears, and poor infrastructure.
However, beyond this crisis, a new model is emerging. Much as remote work decentralised the office, Nigeria might be witnessing the Great Decoupling, a shift from the widespread, strike-prone public giants toward a strike-proof, technology-driven framework of localized care.
A health system under strain: Nigeria’s deepening care deficit
Nigeria’s public health system is buckling under a widening gap between demand and capacity. Despite the 2025 federal budget being branded the “Budget of Restoration,” health sector allocation is ₦2.56 trillion, or just 5.18 percent of total expenditure. This falls well short of the 15 percent benchmark set under the 2001 Abuja Declaration, implying a funding shortfall of nearly ₦4.9 trillion relative to stated continental commitments.
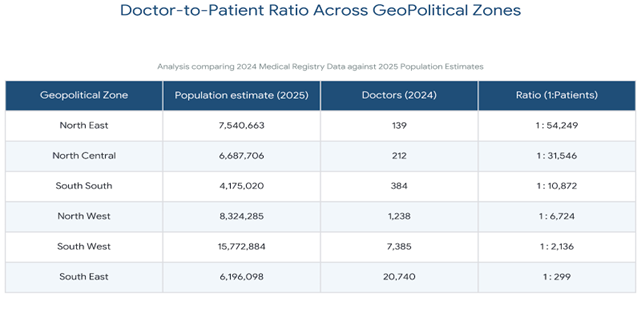
The consequences are most evident in human resources for health. As of 2025, the Nigerian Medical Association estimates a doctor-to-patient ratio of 1:3,500 to 1:5,000, compared with the World Health Organization’s recommended 1:600. This structural shortage is being exacerbated by accelerating medical migration. In 2024 alone, 4,193 doctors and dentists left the country, contributing to an estimated 200 percent surge in outward migration across health cadres.
Industrial actions—such as the ongoing JOHESU strike—compound this fragility by temporarily removing large segments of an already overstretched workforce. For millions of Nigerians, particularly those reliant on public facilities, these disruptions eliminate the last remaining access point to care. In this context, insulating healthcare delivery from recurrent labour shocks is no longer merely a reform ambition—it is a systemic survival imperative for a nation of over 230 million people.
The new decoupled health opportunity
The fastest path to specialist care is no longer found in the crowded, strike-vulnerable wards of teaching hospitals. A new “Decoupled Health Economy” is rising, characterized by compact, specialized Tier-2 hubs.
Investors are moving toward asset-light model centers that focus specifically on high-demand services, such as maternity, renal care, and oncology.
The Nigeria Sovereign Investment Authority (NSIA) has already provided a blueprint for this, launching an expansion program that includes 23 diagnostic centers, three oncology centers, and seven catheterisation laboratories across Nigeria’s six geopolitical zones. These centers act as strike-proof nodes because they are often managed through Public-Private Partnerships (PPPs) or private governance, ensuring they remain operational even when national unions down tools.
The legacy vs. The decoupled model
Nigeria’s vision for a truly strike-proof, decoupled health economy is clear, but major gaps still prevent nationwide scale. The country lacks professionally managed digital health rails and automated diagnostic hubs needed for resilience, especially during system disruptions. When hospitals shut down, patients need remote triage, yet digital access remains uneven.
Platforms like MySmartMedic are helping by combining AI-powered triage with community health workers, but more than 20 million Nigerians still lack internet connectivity, according to the Minister of Communications, Innovation, and Digital Economy, Bosun Tijan, limiting universal access.
At the same time, Nigeria is struggling to retain talent, with over 43,000 health workers eyeing opportunities abroad. Clinicians increasingly prefer workplaces equipped with modern infrastructure and AI-assisted diagnostic tools, rather than outdated, dilapidated equipment that makes their jobs discouraging.
Beyond workforce challenges, the road to recovery depends on building automation and home-based care models that keep the system running even when people cannot. Recent investments, such as the deployment of 73 AI-enabled X-ray units capable of rapid diagnostics without relying solely on human interpretation, show early progress but are insufficient for true continuity.
As more families relocate to emerging satellite cities, the country also lacks a structured “health-at-home” model that integrates remote monitoring with neighborhood-level diagnostic nodes. Until these foundational systems are in place, Nigeria’s health economy will remain vulnerable to strikes and other human-driven disruptions.
Rebuilding Healthcare Nigerians Can Rely On For millions of Nigerian families, healthcare has become an exercise in uncertainty- never fully assured that a hospital will be open when care is most urgently needed. Reimagining the system around a more decoupled model is fundamentally about restoring reliability. Shifting away from overcentralised, strike-vulnerable tertiary facilities toward resilient neighbourhood clinics and digital-first care nodes offers a pathway to continuity, even amid national labour disruptions.
The objective is not simply higher spending, but better transmission: ensuring each naira reaches patients through accessible, always-on services. Technology is increasingly central to this transition. AI-enabled diagnostics and automated triage reduce delays, turning days of waiting into minutes of decision-making. More importantly, they lower the load on overstretched clinicians while improving patient outcomes. This shift also carries strategic value -retaining medical talent, limiting outbound health spending, and rebuilding confidence in domestic care. Policy frameworks are beginning to align.
The Nigeria Health Sector Renewal Investment Initiative (NHSRII) and its Sector-Wide Approach (SWAp) aim to coordinate financing and delivery, but usage trends already signal where momentum lies. Federal Ministry of Health data show visits to facilities supported by the Basic Health Care Provision Fund (BHCPF) rising from 10 million to 45 million by mid-2025, underscoring demand when infrastructure exists.
Sustainability now hinges on building robust Health Rails—the digital and physical systems linking care nodes nationwide. Expanded satellite connectivity via NIGCOMSAT, the $1.7 billion HOPE Project, which is strengthening primary healthcare, and AI platforms such as MySmartMedic and Clafiya, which already manage up to 60 per cent of advisory-level consultations, illustrate how decentralised care can absorb Nigeria’s health burden—if infrastructure keeps pace.
A healthy, balanced way of living
The victory for Nigeria is in the “Great Decoupling.” It is a system where health is no longer a hostage to industrial disputes, but a stable, asset-building infrastructure for every citizen.
By integrating AI-driven diagnostics, supporting Tier-2 specialized centers, and completing the digital health rails, Nigeria can save up to ₦4.8 trillion annually, which the Federal Government is targeting to reap from preventable diseases and retained tourism spend.
Ultimately, this is not just about hospitals; it is about building a strike-proof life. a healthcare system that remains on, even when the rest of the world shuts down.