Universal Health Coverage (UHC) is often framed as a distant aspiration, an ambitious goal to be achieved through long-term planning, global commitments, and incremental reforms. It is frequently imagined as a future utopia in which everyone can access quality healthcare without financial hardship.
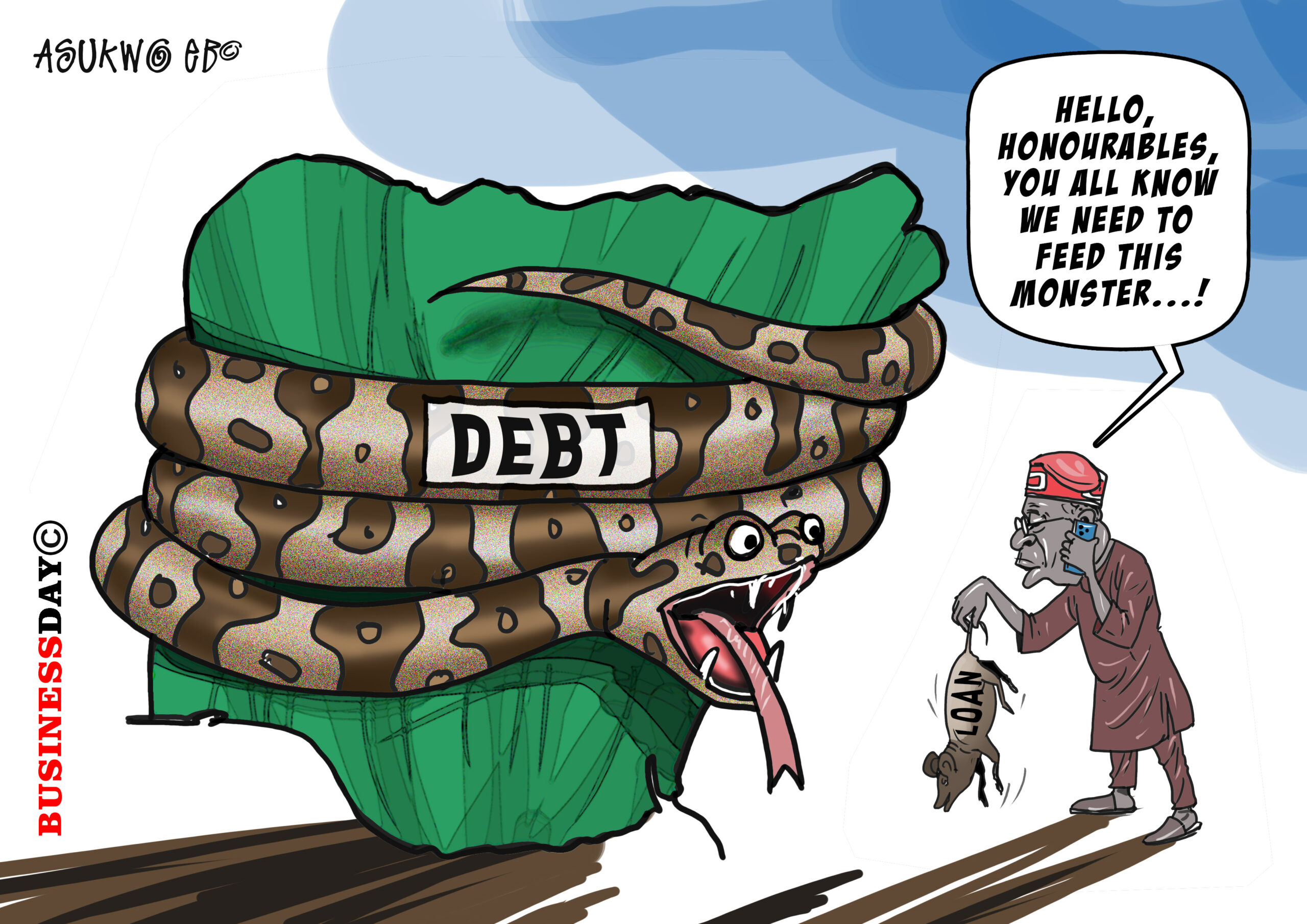
For Africa, however, UHC can no longer be treated as a remote ideal. It is an urgent, present-day necessity for more than 1.2 billion people. The continent’s population is growing at one of the fastest rates globally, while economic pressures (including currency volatility, rising debt burdens, and persistent fiscal deficits) continue to strain already limited public budgets. At the same time, declining donor funding in recent years has further exposed structural weaknesses across health systems.
In Nigeria, the narrative of health system challenges is well known, almost numbing in its repetition, not because the problems are overstated, but because they have endured for so long. Chronic underfunding, weak infrastructure, fragmented service delivery, and heavy reliance on out-of-pocket spending have defined the system for decades. With only about 10 per cent of the population covered by health insurance, millions of Nigerians remain exposed to catastrophic health expenditures that push households into poverty and erode trust in formal care.
Yet within this difficult landscape, a more hopeful and pragmatic pathway is beginning to emerge. This pathway is anchored in strategic collaboration, innovation, and systemic reform, and it offers a realistic route toward UHC. Championing this approach is the Healthcare Federation of Nigeria (HFN), working in close partnership with the National Health Insurance Authority (NHIA) and the Presidential Initiative for Unlocking the Healthcare Value Chain (PVAC). Together, these institutions are advancing not a rhetorical vision of UHC, but a coordinated and actionable reform agenda capable of reshaping Nigeria’s health system over the long term.
Reframing the narrative: The role and vision of the Healthcare Federation of Nigeria
At the core of HFN’s approach is a deliberate effort to change the narrative around healthcare in Nigeria, from one defined by deficits and dysfunction to one focused on opportunity, reform, and shared responsibility. In collaboration with strategic public-sector partners such as PVAC and NHIA, HFN is helping to drive a comprehensive effort to address both the structural and financial foundations of the health system.
Rather than positioning itself narrowly as an advocate for private healthcare providers, HFN is increasingly acting as a systemic integrator. Its work spans policy advocacy, private-sector coordination, mobilisation of investment, support for local manufacturing, and expansion of insurance coverage. Through a series of Memorandums of Understanding (MoUs) signed in recent years, HFN has formalised partnerships that enable practical engagement across the health value chain.
These efforts are designed to bridge the long-standing divide between healthcare supply and demand. On one hand, they aim to strengthen infrastructure, service quality, and local production. On the other hand, they seek to expand financial protection and access through insurance and more efficient financing mechanisms. Together, these reforms are intended to build a more sustainable health ecosystem, one that delivers broad access, reduces financial hardship, and reinforces a strong primary healthcare (PHC) foundation.
Collaboration as strategy: Unlocking Nigeria’s healthcare value chain
A central pillar of HFN’s reform agenda is the transformation of Nigeria’s healthcare system into a more integrated and resilient value chain. This approach recognises that UHC cannot be achieved through isolated interventions; it requires alignment across manufacturing, regulation, financing, service delivery, and human resources.
In recent years, HFN has deepened collaboration with PVAC, NHIA, and regional and global partners to unlock bottlenecks that constrain the health sector. In August 2025, HFN presented a detailed position paper to PVAC, outlining policy and regulatory reforms needed to improve efficiency, reduce costs, and stimulate private-sector investment across the healthcare ecosystem. This was followed, a month later, by a formal agreement between HFN and PVAC to strengthen private-sector participation, promote local pharmaceutical and medical device manufacturing, and catalyse investment in healthcare infrastructure, with support from the World Bank and other stakeholders.
HFN’s approach is informed by regional experience. Ghana’s National Health Insurance Scheme offers lessons on the importance of political commitment and broad enrolment, while also highlighting challenges related to financial sustainability and claims management. Post-Ebola recovery efforts in Sierra Leone and Liberia demonstrate the critical role of community health workers in extending coverage to remote populations.
Meanwhile, Côte d’Ivoire and Senegal illustrate how digital health platforms and public-private partnerships can modernise service delivery and improve system efficiency.
These lessons reinforce the need for context-specific reforms that balance ambition with operational realism.
A dual-axis reform agenda: Supply and demand in tandem
The reform strategy advanced by HFN and its partners is deliberately structured around two mutually reinforcing axes: supply-side strengthening and demand-side expansion.
On the supply side, priority is placed on improving healthcare infrastructure and accelerating local manufacturing. PVAC’s mandate to unlock the healthcare value chain emphasises domestic production of pharmaceuticals, medical consumables, and devices. Expanding local manufacturing is expected to reduce reliance on imports, stabilise supply chains, lower costs, and enhance system resilience, particularly during economic or global supply shocks.
On the demand side, HFN is actively supporting efforts to expand health insurance coverage under the NHIA framework. The 2022 legislation establishing NHIA created a legal foundation for universal coverage across both formal and informal sectors. However, enrolment remains far below national targets. To close this gap, HFN has advocated for a coordinated expansion strategy that combines private-sector insurance delivery with public-sector oversight and targeted subsidies for low-income households.
Addressing both supply and demand concurrently is critical. Expanding insurance coverage without improving service availability risks eroding trust, while investing in infrastructure without financial protection limits utilisation. The dual-axis approach seeks to avoid these pitfalls by advancing reforms in parallel.
A phased roadmap toward universal Health Coverage
To translate reform into measurable progress, HFN has articulated a phased roadmap that moves Nigeria from a fragmented, import-dependent system toward one that is integrated, equitable, and sustainable.
Phase 1 (2025–2027): Strengthening Infrastructure and Supply: The initial phase focuses on upgrading healthcare infrastructure across public and private facilities. Priorities include reliable electricity, access to essential medicines, and strengthened supply chains. In collaboration with PVAC, local manufacturing initiatives will be launched with clear production targets for priority health products. HFN will also work with the National Primary Health Care Development Agency (NPHCDA) to rehabilitate and co-manage PHCs, ensuring that underserved communities benefit from early reforms.
Phase 2 (2026–2029): Expanding Insurance Coverage and Outreach: The second phase emphasises rapid expansion of insurance enrolment. Targeted outreach campaigns will focus on rural populations, informal workers, and low-income households. HFN proposes tiered premium structures and cross-subsidisation mechanisms to improve affordability, complemented by government support through the Basic Health Care Provision Fund (BHCPF).
Phase 3 (2028–2035): Consolidating Gains and Scaling Nationwide: The final phase aims to consolidate gains and scale reforms nationally, with the objective of reaching 40–50 per cent insurance coverage. Robust data systems will be deployed to monitor enrolment, service utilisation, and health outcomes. The private sector will play a central role in maintaining quality standards, transparency, and accountability across facilities.
Economic and health returns on UHC Investment
The anticipated benefits of these reforms are substantial. Nigeria currently relies heavily on out-of-pocket spending, which accounts for approximately 76 percent of total health expenditure. Expanding pooled financing through insurance would significantly reduce catastrophic spending, improve household financial protection, and limit health-related impoverishment.
Health outcomes would also improve markedly. With sustained investment in primary care, preventive services, and chronic disease management, Nigeria could reduce maternal and infant mortality by as much as half over the next decade. Life expectancy would rise, reflecting gains in both access and quality of care.
Local manufacturing as a catalyst for affordability and growth
Local manufacturing represents one of the most transformative elements of HFN’s strategy. In partnership with PVAC, the ambition is to produce up to 70 percent of Nigeria’s health products locally by 2030. Achieving this target would lower costs, strengthen supply security, create jobs, and position Nigeria as a regional manufacturing hub serving West and Central Africa.
Beyond health outcomes, this strategy supports broader economic diversification, foreign exchange generation, and industrial development.
Restoring trust through quality and accountability
Sustained reform depends on public trust. Transparent governance, effective regulation, and strong quality-assurance systems are essential to ensuring that insurance coverage translates into real access and meaningful care. HFN is committed to supporting standards that promote accountability across both public and private providers, reinforcing confidence in the health system.
A call to collective action
Achieving Universal Health Coverage in Nigeria is ambitious, but it is achievable. It requires coordinated action across government, the private sector, civil society, and development partners. By aligning the efforts of HFN, PVAC, NHIA, and other stakeholders, Nigeria can build a health system that is resilient, equitable, and fit for the future. The opportunity to act is narrow, but the potential rewards are profound. With sustained political will, strategic collaboration, and disciplined implementation, Nigeria can secure a healthier future for its people while investing in the human capital that underpins long-term economic growth.
This article is a partnership between the Healthcare Federation of Nigeria (HFN) and BusinessDay to highlight policies and programmes to promote the rebuilding of Nigeria’s health sector. As a private sector-led coalition, HFN advocates for policies and partnerships to strengthen healthcare delivery. This partnership aims to spark meaningful discussions and drive transformative change in Nigeria’s health sector.
This article was developed with input from members of the HFN Editorial Committee, including Njide Ndili (President of HFN and Country Director of PharmAccess), Dr Benson Ayodele-Cole (First Vice President of HFN and CEO of Echo-Scan Services Ltd), Dr Jennifer Anyanti (Second Vice President of HFN and Deputy Managing Director of the Society for Family Health Nigeria) and Dr Folajimi Adebowale (CEO of Recon Health Media).