Marcus Inyama, a medical consultant with the University of Calabar Teaching Hospital, has stated that late diagnosis, not blood transfusion is the real issue surrounding the recent passing away of Esther Mensah.
This clarification is coming at a time when the passing away of Esther Mensah has sparked intense debate on social media, with many focusing on her refusal of blood transfusion.
Inyama however said this narrative overshadows the critical reality: she was battling Stage 4 cancer, a terminal condition.
Medical experts emphasize that blood transfusion is not a cure for advanced cancer. When cancer reaches Stage 4—meaning it has metastasized to distant organs—the prognosis is poor, and treatment goals shift from cure to comfort.
He explained that stage 4 cancer indicates that the disease has spread beyond its original site to other parts of the body, adding that at this point, survival rates plummet. For metastatic breast cancer, the 5-year survival rate is approximately 28 percent (American Cancer Society, 2022), he said.
According to him, treatment focuses on palliative care, aiming to relieve symptoms and improve quality of life rather than reverse the disease.
Cancer: A Global and Local Challenge
According to the World Health Organization (WHO), cancer remains one of the leading causes of death worldwide, claiming an estimated 10 million lives in 2020.
In Nigeria, breast cancer is the most prevalent cancer among women, with a 5-year survival rate of 57 percent (Globocan, 2020). However, when detected late, survival rates drop dramatically.
For metastatic breast cancer, the 5-year survival rate is approximately 28 percent (American Cancer Society, 2022). At this stage, treatment focuses on palliative care—managing symptoms and improving quality of life rather than seeking a cure.
“The issue is not the blood transfusion; it’s the late diagnosis,” says Inyama.
“By the time cancer has metastasized, the focus should be on symptom management and improving quality of life.”
He stated that rather than sensationalizing personal medical choices, the conversation should center on early detection.
“Routine screenings such as mammograms, clinical breast exams, and self-examinations significantly improve treatment outcomes. For localized breast cancer, the 5-year survival rate is 99 percent (American Cancer Society, 2022),” he said.
He called on journalists to wield immense influence in shaping public perception. Instead of amplifying social media debates, they should collaborate with medical professionals to provide balanced, evidence-based reporting.
“Interviews with oncologists, hematologists, and cancer researchers can help the public understand the real challenges—late diagnosis and inadequate screening.
“Let’s shift the conversation from blood transfusion to early detection and prevention,” urges Inyama. “We owe it to our patients and communities to promote health awareness.”
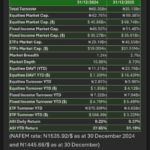
Key Statistics
5-year survival rate for localized breast cancer: 99 percent
5-year survival rate for metastatic breast cancer: 28 percent
Estimated breast cancer deaths in Nigeria (2020): 3,243.
He said the passing of Esther Mensah should serve as a wake-up call—not about blood transfusion, but about the urgent need for early cancer detection and public health education.
“By prioritising awareness and preventive care, we can reduce cancer mortality and improve outcomes for countless lives,” Inyama added.