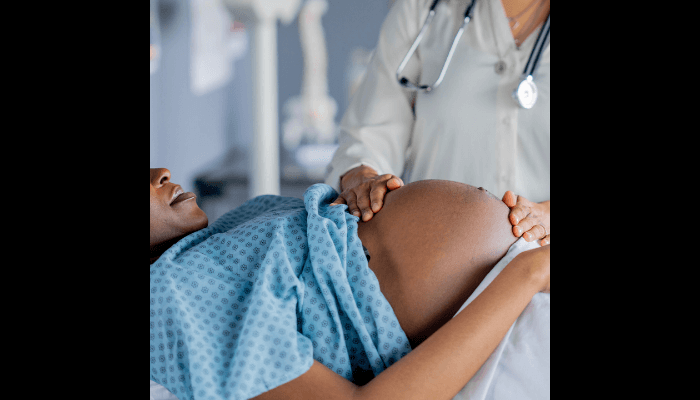
The caesarean section has undergone a quiet but consequential transformation. Once a measure of last resort, summoned only when childbirth crossed from difficulty into danger, it is now edging toward normalcy in many parts of the world. In some countries, surgical delivery has become the dominant mode of birth, scheduled with the precision of a board meeting and justified with the language of efficiency and risk management. Nigeria, however, tells a more fractured and revealing story, one that exposes not excess alone, but inequality, fragility, and the uneasy intersection of medicine, money, and belief.
Globally, the rise has been swift and well documented. In 1990, roughly seven percent of births worldwide were delivered by caesarean section. Today, that figure stands at about twenty-one percent, meaning more than one in five babies now enter the world through an operating theatre rather than a labour ward. Projections suggest that by the end of this decade, nearly thirty per cent of all global births may be surgical, amounting to close to forty million caesarean deliveries each year. In parts of Latin America, Eastern Asia, and the Middle East, national rates already exceed forty percent, while in countries such as Brazil, Turkey, and the Dominican Republic, more than half of all births occur by caesarean section.
“For them, the global debate about “too many caesareans” feels distant, even indulgent. Their reality is not excess, but absence.”
These figures have prompted global concern, not because caesarean delivery is inherently dangerous, but because evidence shows that beyond a certain threshold, rising rates no longer translate into better outcomes. The World Health Organisation has consistently observed that as caesarean rates rise toward around ten percent at the population level, maternal and neonatal mortality decline. Beyond that point, however, the benefits plateau, while the risks and costs continue to accumulate. Surgery saves lives when it is needed; it adds little when it is not.
Nigeria sits well below this global average, but that statistic is misleading if taken at face value. Nationally representative data from recent demographic surveys suggest that approximately six percent of births in Nigeria are delivered by caesarean section. Earlier analyses placed the figure even lower, between two and three percent, making Nigeria one of the countries with the lowest caesarean prevalence in the world. On paper, Nigeria appears untouched by the global surge in surgical birth. But in reality, this low average conceals a profound imbalance in who receives life-saving care and who does not.
The first fracture is geographical. Urban Nigerian women are far more likely to deliver by caesarean section than their rural counterparts. In cities, roughly one in ten births is surgical; in rural areas, the figure falls to about three percent, and in some northern zones, to well below one percent. The second fracture is socio-economic. Women with post-secondary education are several times more likely to have a caesarean than women with no formal schooling. Among the wealthiest households, caesarean delivery approaches twenty percent, while among the poorest, it remains vanishingly rare.
These numbers do not describe a population choosing natural birth over medical intervention. They describe a system in which access to surgery is determined less by clinical need than by affluence, education, and purchasing power. Millions of Nigerian women who medically require a caesarean never receive one. They labour at home or in ill-equipped primary health facilities, far from operating theatres, blood banks, anaesthetists, and reliable electricity. For them, the global debate about “too many caesareans” feels distant, even indulgent. Their reality is not excess, but absence.
Read also: Scars of honour: Why more women are going the cesarean section way
Paradoxically, a different Nigeria experiences the opposite. In tertiary hospitals and private facilities across Lagos, Abuja, Port Harcourt, Ibadan and Onitsha, caesarean delivery is common. Facility-based studies across the country show average caesarean rates of around seventeen to thirty percent, with some teaching hospitals reporting even higher figures. Most of these procedures are emergencies rather than electives, reflecting late referrals and prolonged labour rather than pre-planned choice. Yet the contrast remains striking: where surgical capacity exists, caesarean delivery is frequent; where it does not, women deliver without it, regardless of need.
This dual reality underscores a central truth. Nigeria does not suffer from a uniform rise in caesarean sections. It suffers from a deeply unequal distribution of them. The caesarean section, in Nigeria, is neither normalised nor rare; it is stratified.
The clinical case for caesarean delivery is not in dispute. When medically indicated, it is one of the most powerful tools in modern obstetrics. It prevents deaths from obstructed labour, severe bleeding, placental complications, uterine rupture, and foetal distress. In countries with functioning health systems, it has transformed childbirth from a high-risk event into a largely predictable one. But sadly, Nigeria accounts for nearly 29% of global maternal deaths, with about 75,000 women dying annually from pregnancy-related causes. This stubbornly high maternal mortality ratio would be significantly reduced if timely caesareans were available to all women who needed them.
Yet surgery carries its own burdens. Caesarean delivery is a major abdominal surgery, with higher immediate risks of infection, haemorrhage, and thromboembolism than uncomplicated vaginal birth. Recovery is longer and more demanding. The operation increases the likelihood of complications in subsequent pregnancies, including placenta accreta and uterine rupture, conditions that require highly specialised care. In settings where postoperative monitoring is inconsistent and emergency response is fragile, these risks are magnified.
And beyond the clinical lies the economy. In Nigeria, caesarean delivery is often a financial shock. Health financing remains dominated by out-of-pocket spending, and even in public hospitals, the costs of surgery, drugs, blood, consumables, and informal fees can be devastating. An emergency caesarean can consume months or years of household income. Families sell land, withdraw children from school, or borrow at punishing interest rates to pay hospital bills. Recovery time compounds the damage, particularly for women in the informal economy who cannot afford weeks without income.
For hospitals, the economics are equally complex. In private facilities, caesarean sections are predictable, time-bound, and more lucrative than prolonged labour management. In underfunded public hospitals, surgical fees often subsidise other services, creating quiet incentives to favour such intervention. The danger is not malicious intent but systemic distortion, where financial survival and clinical judgement drift too close together.
Culture exerts its own powerful influence. In many Nigerian communities, vaginal birth remains a measure of strength and moral worth. Caesarean delivery may be interpreted as failure, weakness, or even spiritual affliction. These beliefs shape real decisions. Consent is delayed. Relatives debate. Prayers replace signatures. Time is lost while the mother’s labour worsens and foetal oxygen dwindles. Studies and hospital accounts repeatedly link delayed consent to poor outcomes, yet the stigma persists.
At the same time, an opposing narrative is emerging among Nigeria’s urban middle and upper classes. Here, caesarean delivery is increasingly framed as control and foresight, a way to manage pain and risk in an environment where unpredictability carries high costs. It fits neatly into rigid work schedules, limited maternity leave, and the pressures of professional life. Nigeria is thus holding two conversations about birth at once, divided sharply by class and economics.
The health system absorbs these contradictions at great cost. Expanding caesarean capacity requires sustained investment in operating theatres, anaesthesia, blood services, infection control, power supply, and skilled personnel. Where these investments are made, outcomes improve. Where they are not, surgery becomes a dangerous promise. Nigeria’s maternal mortality crisis is not evidence that caesareans are unsafe; it is evidence of what happens when surgical care is uneven, delayed, or poorly supported.
Compared with global trends, Nigeria’s challenge is not to reverse an excess but to correct a misallocation. While high-income countries debate how to reduce unnecessary caesareans, Nigeria must still ensure that women who need surgery can access it without stigma, delay, or financial ruin. The risk is that global narratives about “too many caesareans” obscure the far more urgent Nigerian reality of too few, delivered too late, to the wrong people.
The policy response must therefore resist false choices. Nigeria does not need campaigns that romanticise natural birth at the expense of safety, nor does it need unchecked expansion of surgical delivery driven by fear or profit. It needs precision and equity. Caesareans must be timely and affordable when medically indicated and discouraged when unnecessary. This requires stronger antenatal risk screening, functional referral systems, emergency transport, and consistent clinical audit. It requires financial protection mechanisms that prevent childbirth from becoming a household catastrophe. And it requires public education that dismantles stigma without turning surgery into a lifestyle aspiration.
In a world where caesarean birth is fast becoming the norm, Nigeria’s task is more exacting. It must ensure that surgery is neither a privilege of wealth nor a symbol of failure, but a dependable medical option available when life demands it. Progress will not be measured by rising or falling percentages, but by whether a woman in labour can expect competent care without bargaining for survival. That is the curve Nigeria must bend, and the only statistic that truly matters.
Dr Hani Okoroafor is a global informatics expert advising corporate boards across Europe, Africa, North America, and the Middle East. He serves on the Editorial Advisory Board of BusinessDay. Reactions are welcome at doctorhaniel@gmail.com.