Despite spending more than $1 billion every year on drugs, insecticide-treated nets, diagnostics, and public health campaigns, malaria remains deeply entrenched in Nigeria, a paradox experts at the Nigerian Institute of Medical Research (NIMR) attribute not to failed science but to biological resistance, environmental conditions, human behaviour, and weak implementation gaps.
Prof. Muhammad Ali Pate, Nigeria’s coordinating minister of Health and Social Welfare, , has estimated the economic burden of malaria at between $1.1 billion and $1.6 billion annually in healthcare costs and lost productivity, warning that the figure could rise to $2.8 billion by 2030.
Pate noted that the disease drains household incomes through high out-of-pocket spending while slowing national growth by reducing workforce productivity and discouraging tourism and investment.
This is even as health officials at NIMR say the burden falls heaviest on vulnerable groups, particularly children and rural workers, as families spend on treatment and lose income to illness.
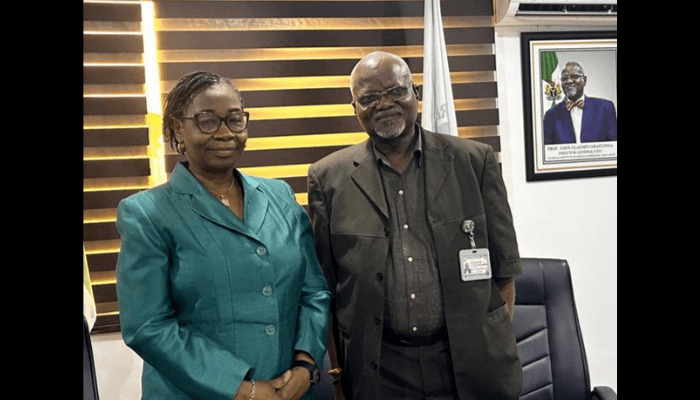
Dr. Adeola Olukosi, director of research and head of NIMR’s Malaria Research Group, at a media chat organization by the Institute in Lagos, explained that resistance, both by parasites to drugs and mosquitoes to insecticides is inevitable.
Read also: Over 200,000 Nigerian children receive new malaria vaccine – NPHCDA
“Drug resistance by parasites and insecticide resistance by vectors have been with us for a very long time. We have a limited number of drugs and insecticides in our arsenal, and the pressure we apply will always drive resistance,” Olukosi affirmed.
NIMR, in partnership with the National Malaria Elimination Programme (NMEP), conducts continuous surveillance across multiple parasite and vector sentinel sites nationwide to monitor drug efficacy, mosquito behavior, and insecticide susceptibility. Current evidence shows that Nigeria’s recommended artemisinin-based combination therapies remain effective, which is why there is no immediate plan to change national treatment policy.
Olukosi warned against continued use of banned drugs like chloroquine, adding that, “Individual success with such medicines sustains resistant parasite populations and undermines public health gains.”
One emerging strategy reshaping malaria control is Artificial Intelligence (AI). During a large-scale campaign in Kaduna State, AI tools guided evidence-driven interventions, tracked implementation in real time, and identified gaps instantly. “AI helps us see what has been done, where it has been done, and what still needs to be done. We are still using it at the periphery, but it is already improving efficiency,” she said.
Nigeria’s diverse mosquito population adds another layer of complexity. Vectors differ not only across regions but sometimes within the same community, responding differently to control measures. Recent surveillance confirmed the presence of Anopheles stephensi, an invasive mosquito species from Southeast Asia that thrives in urban environments and resists multiple insecticides, raising new challenges for malaria control.
Environmental and biological factors further complicate elimination efforts. Nigeria’s climate, rainfall, vegetation, and abundant breeding sites create ideal conditions for transmission. Human genetics, particularly the sickle cell trait, provides partial protection but allows both the parasite and the gene to persist over time.
Read also: FG, Lagos partner to fight malaria
On funding and sustainability, Olukosi acknowledged that malaria research in Nigeria still relies heavily on external grants, though political commitment is improving. She stressed the importance of domestic ownership of malaria control programs, from research to tool development, and the ethical responsibility to share findings with affected communities.
“We do not do research for research sake. We go back to the communities, explain what we found, and share what can help them,” she added.
She agreed that malaria control cannot succeed without broad collaboration. Scientists generate evidence, but government, media, communities, and individuals all play critical roles. “Malaria is everybody’s problem, and everybody has a role in the solution,” Olukosi said.
Professor John Oladapo Obafunwa, director general of NIMR, cautioned against oversimplifying Nigeria’s malaria statistics, adding that, “Nigeria represents a significant proportion of Africa’s population, so absolute numbers will always appear high. But that does not mean we do not have a serious problem.”
He highlighted that malaria trends in Lagos cannot be directly compared with cities in Europe or North America due to differences in environment, housing, infrastructure, and population movement.
“People move, trade, worship, and travel. Malaria crosses borders with them. Social and behavioral factors, including misdiagnosis, delayed treatment due to poverty, and gender dynamics limiting access to care, also sustain transmission. Not every fever is malaria,” he noted, adding that, misdiagnosis delays appropriate care and distorts our understanding of disease burden.
While Lagos State has reported malaria prevalence as low as two per cent, Obafunwa emphasized that suppression keeping malaria very low and controlled is achievable.
Despite hundreds of millions of insecticide-treated nets and antimalarial drugs distributed over the years, gaps remain in usage, diagnosis, and follow-through. Power outages, housing conditions, delayed care seeking, self medication, and reliance on unverified treatments sustain transmission and resistance patterns.
Obafunwa noted that malaria is often overdiagnosed, masking other illnesses and weakening trust in interventions, adding that, “For years, every fever was called malaria. If you do not test properly, you treat wrongly and the real disease progresses.”
Integrated approaches are crucial, including larval source management, improved housing, environmental sanitation, and targeted protection for high-risk populations. Success depends on domestic ownership, political commitment, and behavioral change. “We cannot outsource our health security. If others fund the research, manufacture the tools, and define the pipeline, then we will always be reacting instead of leading.”
There is no silver bullet. Malaria control requires multiple tools, used intelligently, backed by surveillance, and supported by communities.
While malaria will not disappear overnight, sustained investment, smarter deployment of tools, behavioral change, and collective responsibility can weaken its grip. “Malaria is not just a medical issue. It is social, environmental, economic, and behavioral. Until we address all of these together, malaria will continue to persist,” Obafunwa said.
For NIMR, the fight against malaria begins not only in laboratories and hospitals but also in homes, communities, and everyday choices.