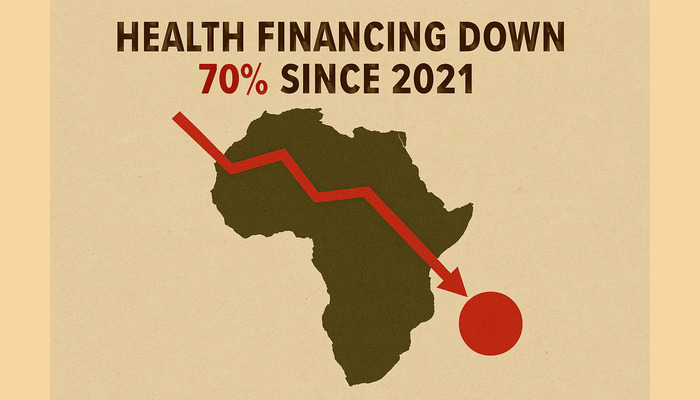
Africa is accelerating a sweeping shift toward domestic health financing as donor support for the continent’s health systems collapses, with official development assistance plunging 70 percent since 2021.
Confronted with rising outbreaks, severe funding gaps, and mounting global uncertainties, African governments, under the leadership of the Africa Centres for Disease Control and Prevention (Africa CDC), are moving to strengthen self-reliance through a new Health Security and Sovereignty (AHSS) agenda that aims to end decades of dependence on foreign aid.
The new framework, outlined by Dr. Jean Kaseya, Africa CDC director in a Lancet comment, marks one of the most far-reaching responses to the post-pandemic decline in global health financing. It seeks to reposition the continent from vulnerability to resilience at a time when disease outbreaks have surged by 41 percent between 2022 and 2024 and climate pressures are intensifying health risks.
“Without predictable domestic financing and stronger systems, Africa risks losing decades of progress,” Kaseya warned, saying the continent must no longer rely on emergency goodwill or external supply chains when new epidemics emerge.
Read also: Financial institution, providers back Lagos Private Health Partnership initiative
At the heart of the AHSS agenda is a strong push for African countries to take greater ownership of their health budgets through predictable domestic, blended, and innovative financing models. The plan aligns with the Lusaka Agenda, which advocates increased national spending, improved public financial management, and new revenue-generating instruments such as solidarity levies, diaspora bonds, and health taxes.
Africa CDC’s target that at least 50 percent of Africa’s health-security financing should come from national budgets, reducing dependence on external partners and easing the burden on households that currently face some of the highest out-of-pocket health expenditures in the world.
However, major governance bottlenecks remain. Kaseya highlighted persistent procurement fraud, the prevalence of ghost workers, fragmented planning, and poor digitalisation as structural weaknesses that continue to undermine health budgets.
Read also: Nigerian newsrooms face mental-health crisis, psychiatrist warns
To address this, Africa CDC is deploying Public Finance Management Specialists to member states to support budgeting reforms, expenditure tracking, and accountability. “These steps are essential because there will be no health sovereignty without innovative domestic resources,” he said.
The AHSS agenda also introduces a permanent, continent-wide mechanism for pandemic prevention, preparedness, and response (PPPR). The newly institutionalised Incident Management Support Team (IMST) consolidates expertise, surveillance systems, laboratories, and emergency response teams into a unified operational structure that is always active, rather than assembled only during crises.
This model, tested during mpox, cholera, and Marburg outbreaks, is backed by the Africa Epidemics Fund (AfEF), designed to provide emergency zero-day financing and surge support without donor conditions or delays.
Africa CDC argues that a continent of 1.5 billion people cannot afford slow, donor-driven emergency responses. The new PPPR system is intended to ensure rapid detection, response, and containment, long before outbreaks escalate into regional or global threats.
Recognising the financial and strategic burden created by importing over 90 percent of its medical supplies, Africa is also investing heavily in local production. The AHSS agenda sets a transformative target: 60 percent of vaccines, diagnostics, and therapeutics used in Africa must be locally produced by 2040.
The African Medicines Agency, the African Pooled Procurement Mechanism, Afreximbank, the African Development Bank, and other partners are positioned to support regulation, market shaping, and financing for this manufacturing push.
In parallel, Africa CDC is rolling out a continent-wide digital transformation programme, including a Primary Healthcare Digital Intelligence Ecosystem, a Digital Birth-to-Care Card, and a newly signed MoU with Starlink to connect remote health facilities. These initiatives aim to strengthen data accuracy, reduce leakages, improve service delivery, and safeguard Africa’s health data sovereignty.
Africa CDC acknowledges that obstacles remain, from low national health allocations and workforce shortages to misinformation and global intellectual property restrictions that complicate local manufacturing. But Kaseya insists that strong political will and continental integration can overcome these barriers.
“Africa’s vision is not isolationist. It is a call for shared responsibility where Africa leads with clarity, and global partners support, not dictate, our priorities,” he emphasised.
With donor funding shrinking and the burden of outbreaks rising, Africa’s pivot to domestic health financing is not just strategic, it is rapidly becoming indispensable. The continent is betting that deeper investment in its own systems today will secure its health sovereignty, strengthen resilience, and protect millions of lives tomorrow.