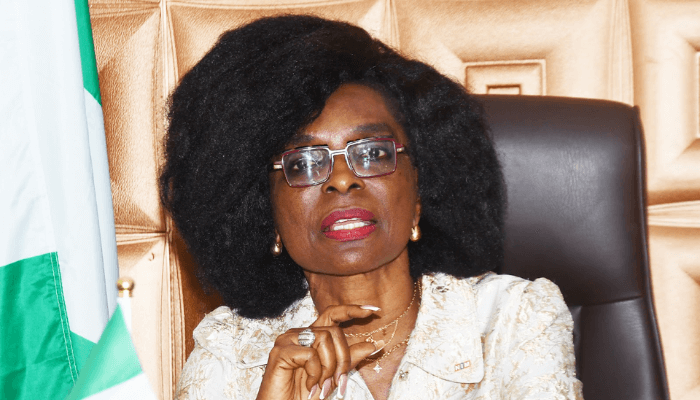
Emem Omokaro is the Director-General of the National Senior Citizens Centre (NSCC), the first federal agency established by law to design and implement cross-sectoral programmes aimed at integrating older persons into national development and enhancing their quality of life.
She holds a PhD in Development Sociology, a Post-Doctoral Certificate in Social Gerontology from the University of Calabar and a Post-Doctoral Certificate in Social Gerontology from the University of Malta. In this interview with the BusinessDay’s Abuja team led by John Osadolor, Managing Editor; Onyinye Nwachukwu, Abuja Bureau Chief; Geofrey Essien, Assistant General Manager, Advert; Anthony Ailemen, Senior Correspondent; and Ladi Patrick-Okwoli, she spoke about her vision for NSCC, which includes advancements in the field of ageing, including the development of the National Policy on Ageing, the country’s first National Strategic Roadmap on Ageing (2022–2032), and the inaugural National Plan of Action on Ageing, alongside capital projects embedded in Nigeria’s National Development Plan.
Talk us through the mandate of NSCC?
First and foremost, the NSCC was established by 2017 legislation. However, the board and appointments were only inaugurated in June 2021. But if you look at the time it took for the take-off grants, establishment of an office, and the actual roll-out of activities, NSCC became effectively operational in 2022. So we have been seriously functioning since then till date, but I can tell you that during these years, including 2021, there were no budgetary provisions. However, the NSCC has accomplished a great deal. First, we had to lay the foundational framework because, as a pioneering agency, there was absolutely nothing on the ground. We had to take the NSCC Act and translate it into a clear vision and mission and then the commitment that the Act portends. At the time of our inauguration, the National Policy on Ageing was also launched. It’s a policy which we helped to draft from scratch while we were working with the government as non-governmental actors. We had to take that policy and operationalise it into a National Plan of Action on Ageing. As a pioneering agency, it was essential to establish systems, institutions, engagement mechanisms, and programmes. This was our focus in 2021 and 2022. During this period, we developed a 10-year Strategic Roadmap on Ageing, which outlines the key challenges and the strategies to address them and identifies the relevant partners and potential funding sources. This 10-year strategic roadmap clearly defines the direction Nigeria is taking in this area. Furthermore, for the first time in our country’s history, the National Plan of Action on Ageing was integrated into the National Development Plan. This marked the first time that senior citizens in Nigeria were included in capital projects under the National Development Plan, with budgetary appropriations made for them.
In terms of what we offer older people, the first major thing, as directed by the policy and outlined in our strategic roadmap, is to make Nigerians understand and develop a positive perception of aging and older persons. Our goal is to reshape the public perception of aging. Currently, many Nigerians see ageing and older persons as a burden, people who are retired and should step aside. Though traditionally, we respect older persons, we must ask: what is happening now?
One of our major programmes is elder justice advocacy. This means advocating against the abuse of older persons, whether verbal, physical or rooted in misunderstanding or misperceptions about ageing. We also advocate for ageing mainstreaming, ensuring that nearly all Ministries, Departments, and Agencies (MDAs) involved in human capital development include older persons in their programmes. Whether it is primary health care, the ministry of health, tertiary institutions, housing, transportation, the National Directorate of Employment (NDE), SMEDAN or any agency delivering services to Nigerians — all must include provisions for older persons. Our aim is to integrate them into existing programmes. For instance, why should primary healthcare services, especially in rural areas, exclude older persons when it is the first point of contact for many?
We have developed programmes and formed partnerships to address this. As I speak, we have established ageing desks in 40 MDAs through high-level advocacy. Each has at least two trained middle-level officers designated as aging desk officers to build institutional relationships. We have created a platform that connects these officers, ensuring coordination and visibility. When addressing ageing, mainstreaming and elder justice advocacy, we take these issues seriously because they relate to the dignity, inclusion and rights of older persons.
We also run income empowerment programmes under the broader theme of income security, tailored to the different realities of the ageing population. On one hand, you have active older persons like myself who still work and contribute to the labour market. This group includes those living in communities, such as traditional artisans and small business owners. We support them by assessing their needs, building their capacity and providing training in local languages. After positive results from our monitoring and evaluation, we formed senior-led multipurpose cooperatives and began empowering them through structured frameworks.
We also include older persons who, due to frailty or extreme age, can no longer earn an income. Although it falls outside our direct mandate because we don’t have a budget for it. So what we do is to advocate for their inclusion in the National Social Investment Programme, such as the unconditional cash transfer managed by the National Social Investment Agency and the National Cash Transfer Office. We compile and forward names through our ministry, which is the Ministry of Humanitarian Affairs, especially those already listed in the National Social Register. We will continue to advocate for old-age grants for the most vulnerable older persons, those who have no income and no support system. That remains a major area of advocacy for us. In terms of income security, we are actively empowering rural older persons. Recently, I was in Akwa Ibom State, where we empowered a senior-led cooperative. This year, we plan to support many more, as it is included in our budget.
Another key area that we focus on is healthy ageing promotion, which includes medical outreach programmes and the distribution of assistive devices. We have conducted these initiatives in nearly all the states. We developed a framework for healthy ageing with the help of partners like primary health care, traditional rulers, and religious organisations. We developed a framework that is sector-wide and all-inclusive. Then we trained and retrained people as volunteers; we also have stakeholders through a consultative forum across states. Now, having piloted the programme in some states, we are giving out grants – ‘Healthy Ageing Promotion Grants’. On April 15, we rolled it out in 18 states. What we do there is to bring old persons and engage them in what we call ‘Work for Life’. Whatever form of exercise they participate in is assessed and approved by medical personnel to ensure that it is safe for them. Then, we offer disease prevention education. We also provide chronic condition management education, nutrition education and medical outreach. During the outreach, there are health assessments, medication dispensing and treatment. For all those who need assistive devices, wheelchairs, hearing aids and glasses, we provide them free of charge. We do this across the country through the grant. This has been a meaningful investment for us. Some old people come to the venue crawling; imagine them being lifted and placed in a wheelchair, making them able to move again, that sense of independence and dignity. The tears they shed, the joy for our staff, everyone cries with them. It brings us so much pleasure to carry out this exercise. We target older persons through our needs assessment. We also target them through our general disseminated data in states – in terms of number, location, etc.
How is your geriatric social care programme addressing the declining traditional family caregiving?
The geriatric social care pertains to building a long-term care system. In Nigeria, as all of us are aware, we traditionally depend on older children to take care of family members. So, it is the family that cares. If you have a sick mother-in-law or father-in-law, it is your responsibility to care for them. But we also know that global trends have changed and family strength has been compromised. All of us are in Abuja, and I am sure most of our parents are in rural areas. So how do we care for them? We end up leaving them in the hands of minors. Some are left with people who have no clue about what they are going through or how to manage their medications. Our aim in the geriatric social care sector is, first, to strengthen families to care better. How do we do that? It is by training and certifying carers so you can call on a carer who is skilled. We took the time to build and are still building the geriatric social care quality assurance system. We have a strong partnership with the National Board for Technical Education, NBTE (the regulators of skills, education and vocational training), and Skills Nigeria Limited. First, we developed the National Occupational Standards, the minimum curriculum to train and certify carers. Nigeria never had anything like that, but now we do.
Then, we established the National Skills Sector Council (NSSC), just like in other sectors. We also have training providers. These include state and federal university hospitals with geriatric units, as well as federal medical centres with geriatric units. We have worked with them. But for them to be accredited to train and certify careers, a good proportion of their multidisciplinary teams must have quality assurance certification, because this is competency-based training, not just lecturing. You must have internal assessors who can determine, for example, “This person trained in Level One can or cannot do what Level One requires.” So they must be assessed based on competency in real work environments. Fortunately for us, teaching hospitals were cooperative. They were not territorial about it. So far, eight state and federal university hospitals got their teams trained during an 11-week intensive training and became certified. They met the major requirements for accreditation. As it stands now, the University of Benin and University of Uyo Teaching Hospitals have been accredited. We also received a special expression of interest from the Federal Medical Centre in Keffi to be accredited. Uyo has finished and wants to be fully accredited. Many institutions are lined up for accreditation as training providers. We now have training providers, and the NSCCs are already operational. For the first time in Nigeria, we are building a geriatric social care system. We are going to produce a skilled workforce. We are also bringing sanity and standards to care facilities. We now have a centralised database and a shared platform.
We are focusing on training and capacity enhancement based on what we have developed. We now have minimum benchmarks and standards for the accreditation of care facilities. These facilities must understand our National Policy Guidelines for Geriatric Social Care and our Standard Breaching Procedures. They must comply. We are working with the National Assembly to pass regulations because you need laws in this field to ensure compliance. So, many things are happening in this space, all for good. In Nigeria, we can now say that we are developing a skilled workforce. It is no longer an all-comers affair. What does this do? It opens up the care economy. Instead of our sons and daughters walking around doing odd jobs, those with interest in this area can train and be certified as carers, not to ‘japa’, but to serve locally as professional carers.
Does the agency have a budget allocated for this?
We are funded through allocation, but it is not enough compared to the scale of work we do nationwide. Even people who are familiar with my ministry often wonder how we manage to accomplish things. The privilege is that I have been in this field long before I became the director general. I have worked with the United Nations and the African Union Commission, and we had a very good foundation. So, as soon as I assumed office, we developed a strategic roadmap. Interestingly, it was vendor-funded. All our stakeholders participated—flying in and out for consultations. The National Plan of Action that you have seen was developed by the United Nations itself. Even our Care Quality Assurance System was established with the help of international consultants, whose travel, accommodation and work were fully funded by our partners. So far, we have had about nine or ten international consultants. Many of them, as it turns out, are Nigerians. So, while we may not have all the funding we wish for, what we do have is immense goodwill. It is because of the way we approach our work—the systems we have built, the institutions we have established, the policy framework and the engagement mechanisms. You would think we have physical offices in every state, yet we don’t. Still, we are present and active across the entire nation.
Recently, we rolled out stakeholders’ consultative fora in 13 states. This is a solid governance structure powered entirely by volunteers. These fora cut across eight major stakeholder categories: national union of pensioners, associations of older persons, and various professional and market associations. We even have representatives from the traditional institutions. We include food-based organisations and ageing experts—physiotherapists, nutritionists, professors and researchers. The private sector and civil society are also well represented. Community-based organisations and NGOs focused on health, nutrition and human rights have been especially formidable in every state. Our governance structure is designed with influence and effectiveness in mind. Each forum has two co-chairs. These are not social media influencers; they are people of deep societal influence—people who can pick up the phone and call top government officials directly. When I ask, “How can I see the Sultan?” they reply, “When do you want to see him?” And they make it happen. These are informal but powerful citizens who play key roles. Our stakeholders range from permanent secretaries and diplomats to grassroots volunteers.
Just recently, I came back from a state where we launched our Healthy Eating Promotion campaign. It was one of the states I personally selected. We provided grants to stakeholder groups there, and even though the grant could not cover surgeries, many of the experts involved—doctors—chose to perform the surgeries free of charge. They called me to the theatre, and I was truly impressed by their volunteerism. The passion and organisation behind this initiative are outstanding. I can stay in the very place where I was born, and through the system we have built, we can reach and impact the entire country. I have engaged with states like Borno, Sokoto, and Zamfara—we are receiving detailed reports from them. We just concluded our Healthy Eating Promotion, and all the reports are coming in—most of which we carried out ourselves. I discussed this with my minister, who was on the ground as well, even in my grandmother’s state. He was astonished and asked how we manage all of this. The answer is simple: it is the engine we have built. A system built on goodwill, volunteerism and inclusive structures. The people enjoy the work; they find fulfillment in it. This is the second time we are awarding grants, and they are competitive; the best ideas win. This last round was one of such grants, and we are preparing to roll out the next phase.
Tell us more about the Geriatric Social Care System.
The geriatric social care system that we are developing has been deliberately structured in phases. The first step was to define the system: establish clear policy directives, set up national benchmark minimum standards and outline national occupational standards. This way, before engaging service providers or practitioners, we already have a defined framework to guide them. We worked closely with the Nigerian National Qualifications Framework to identify the key actors in this space—those whose capacity we need to build to make the system functional. Our focus has been on training providers—not just teaching hospitals, but institutions and private practitioners. These providers must go through our Quality Assurance Accreditation (QAA) process. Without it, they cannot be accredited. We are currently preparing to launch the second batch of QAA training and certification, involving nine states and federal universities, as well as several private sector practitioners. In addition to training providers, we have focused on building the capacity of the regulatory council. This was a foundational step in ensuring that the system has technical and institutional integrity.
A key aspect of the model we are promoting is domiciliary care—which allows older persons to age in peace, within their homes, while care services are delivered directly to them. To support this, we created a national database of domiciliary care providers. Our first major workshop in this area was international in scope, designed to expose providers to global and local best practices. This year, we plan to deepen that work. One of our priorities is to take over the facilities known as “old people’s schools”, which currently fall under the purview of the Ministry of Social Development. We have already developed the necessary system and framework, and we are in ongoing discussions with the ministry for the official handover. Once that happens, we plan to use those facilities as pilot sites to demonstrate how our standards can be implemented—whether in environmental modification, staff training or the certification of care providers. This update is also meant to encourage private sector actors to see the system we are building and understand the opportunities for engagement. So, moving forward, much of our efforts this year will go into capacity enhancement and standardisation in this critical area of geriatric care.
With your deep understanding of how things work in your field, what has been your advice to the government?
Like I said, the population and experiences are diverse. There are some people throughout their lifetime who were faced with the accumulation of negative trajectories. So they knew about poverty for a long time. And some do not have families at all. At their age, they get stranded. They don’t have homes. They are on the streets. By cultural orientation, we are used to taking care of our loved ones. In fact, they would even say, If you do not take me out of here, I will curse you from my grave. So, we are averse to doing that because it is rejection, abandonment and all that. For domiciliary care, this means your older person is in the house, but you are not going to have members of the family who will be in the house 24-7. Most likely, if you force members of the family to be there because of carers, they will start abusing the older person, and you know that about 90 per cent of abuse comes from family members. So what NACSS has done is to develop the geriatric social care skills sector where we train and certify carers at all levels. This training is really intense, so they know communication, ethics, law, and medication management at different levels. We are bringing back our retired nurses, and we are about to sign a Memorandum of Understanding (MoU) with the health extension community.
So they will run the domiciliary agencies, and because of their experience, the trained and certified carers will be under their supervision. There are many Nigerians abroad that are tired of sending money to family members to take care of their parents.
How are you partnering states in all these?
First and foremost, the Act states that state governments should domesticate it and also establish the state senior citizens’ centre. One way we work with states is through high-level advocacy. We go there and work with stakeholders to advocate that the act should be domesticated. Our first target is to ensure that they domesticate the act. As I speak with you, five states have domesticated this act: Kebbi, Cross River, Abia and Kogi. This was achieved through the efforts of our stakeholders, and then some states also developed policies.
Cross River State has a technical committee that we helped them to set up. We also facilitate training, capacity enhancement and policy development. There is one international training that is going to take place in about five states.
Is your agency also working to facilitate the speedy release of their pension?
Yes, we are careful in how we proceed. However, our mandate also includes advocating for our senior citizens. Justice cannot truly be served without at least a brief acknowledgement of their needs and rights. So, whenever we go into the field, we understand that we are automatically assuming an extension of duty. As long as I do not see myself as disrupting any other government agency, I know I am standing in judgement with integrity and not interfering with the responsibilities of another agency. I say this as a representative of a federal government agency: the real challenge lies in local systems that often resist implementing the kind of policies and structures that are necessary at the federal level. That is why advocacy is so important in our work. We stand for those individuals, particularly seniors, who need a voice in the system.